Thank you for Subscribing to Eldercare Review Weekly Brief
The Connection Between Nutrition and Memory Wellness
By
Eldercare Review | Tuesday, June 10, 2025
Stay ahead of the industry with exclusive feature stories on the top companies, expert insights and the latest news delivered straight to your inbox. Subscribe today.
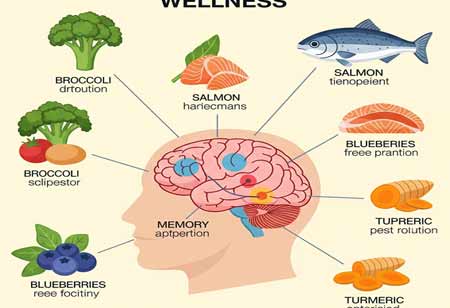
FREMONT, CA: The quality of a person’s diet not only supports physical health but also plays a vital role in brain function by helping to build and maintain neural connections. In individuals with memory disorders, several factors can contribute to poor nutrition, including changes in appetite and taste preferences, increased restlessness and physical activity, difficulty recognising food, challenges with chewing and swallowing, and memory lapses that cause them to forget meals or believe they’ve already eaten. Top memory care communities recognise that nutrition in memory care is about more than just slowing cognitive decline—it’s essential for enhancing overall quality of life. Proper nourishment supports dignity, promotes independence, and provides comfort, making it a key component of effective memory care. With the correct nutrition, there is potential for improvement in cognitive function, instilling hope and motivation in caregivers.
Specific key nutrients play a vital role in supporting brain health, particularly in individuals receiving memory care. Minerals like magnesium help regulate neurotransmitter activity and promote neuroplasticity, while zinc is essential for neuronal differentiation and the formation of synapses. Iron supports critical neural functions such as myelination and dendritic arborisation, and calcium aids in the secretion of neurotransmitters by neurons. The Mediterranean diet, which is rich in these nutrients, has been shown to reduce cognitive decline and lower the risk of neurodegenerative diseases. By emphasising vegetables, fruits, olive oil, and fish, this diet provides comprehensive brain nutrition that supports cognitive function and overall well-being. Caregivers who understand the importance of this diet can make informed decisions about their loved ones' nutrition, feeling knowledgeable and empowered in their role.
Dietary Challenges in Seniors with Memory Disorders
Seniors with memory disorders face a range of eating challenges that worsen as cognitive decline progresses. One of the earliest signs is unintentional weight loss, often caused by forgetting meals or believing they’ve already eaten. Physical difficulties, such as trouble chewing, swallowing, using utensils, and recognising food, further complicate proper nutrition. Sensory changes, including diminished taste, smell, and vision, can make food less appealing or even hard to identify on a plate. Many also begin to prefer sweet or intensely flavoured foods, such as ice cream, chocolate, or heavily seasoned dishes, leading to unbalanced diets. Additionally, side effects from medications—especially those used to treat Alzheimer’s—can suppress appetite and contribute to undernutrition.
Hydration and Its Impact on Cognitive Function
Water is essential to brain health, making up about 75 per cent of the brain’s mass. Even slight dehydration, as minor as a 2 per cent loss in body fluids, can impair focus, memory, and reaction time. This is especially concerning for seniors with memory disorders, who often have a diminished sense of thirst, increasing their risk of dehydration and cognitive decline. Dehydration can lead to noticeable changes in the brain, including a 0.55% reduction in brain volume after just 16 hours without water, expansion of ventricular spaces, heightened BOLD responses during mental tasks, and a decline in working memory.
As memory disorders progress, maintaining proper dietary habits becomes increasingly challenging yet even more critical. Caregivers, by prioritising brain-healthy diets, such as the Mediterranean diet, and ensuring adequate intake of essential nutrients and fluids, play a vital role in mitigating the effects of cognitive decline and promoting long-term neurological health. Their role is not just supportive, but integral to the care process.






